One of my two articles in the November issue of Nature Biotechnology looks at some of the cool stuff that’s going on right now with wearable wireless medical sensors that can track and transmit data about cardiac health, blood sugar and even brain activity to a smart phone for the benefit of patients, their family members and their caregivers.
Among the most commonly cited challenges in bringing these tools forward is providing adequate power to drive both the device and to enable routine data transmission to ensure that the wearer is getting a real-time ‘story’ of physiological changes. We all know that even while technology just gets more powerful and versatile, batteries have more or less continued to suck, and the folks who have been trying to create fully functional medical devices that are essentially small enough to be taped onto your body with a Band-Aid have really been grappling with this. Julian Penders at Belgium’s IMEC research institute is deeply immersed in the world of so-called ‘body area networks’, the design of wireless electronics for physiological monitoring, and a lot of his team’s efforts are particularly focused on this problem and in particular on the idea of moving away from conventional batteries altogether. He told me:
“There has been quite a lot of work in terms of energy harvesting… the dream is to have wearable devices that can be used for an entire lifetime without having to charge them. We’ve been looking into thermal harvesting, radiofrequency harvesting and harvesting of energy from vibrations. We’re not at the point where we can have a fully autonomous system, but I would say that the gap between consumption and generation and harvesting of power is really shrinking. We are on the order of 1 milliwatt for a wearable electrocardiograph, and what we can generate in terms of harvesting is typically on the order of around 100 microwatts – we still have a factor of ten to bridge, but this gap has become much easier to cross.”
Obviously, this is really cool stuff – the equivalent of a body-powered ‘perpetual motion machine’ (or at least as perpetual as things get for we mere mortals). Plus, it’s just one less thing to worry about when your doctor is worried about making sure your heart is working properly 24/7.
If only I’d been able to wait another month! Just in the past week, a pair of research teams have presented two completely different mechanisms for continuously harvesting power to drive an on-body medical device. The first of these appeared in the exact same issue of Nature Biotech as my article.
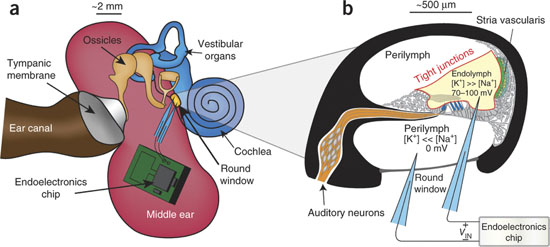
MIT’s Anantha Chandrakasan and Konstantina Stankovic of the Massachusetts Eye & Ear Infirmary took advantage of a source of natural electrical power within the inner ear. The cochlea is a snail shell-shaped structure where vibrations received at the eardrum get translated into neural impulses to the auditory cortex of the brain. It contains two types of fluid with different ionic concentrations, separated by a membrane, resulting in a voltage potential of 70-100 millivolts. This endocochlear potential (EP) is a critical component for the generation of electrical signals in response to sounds and therefore must be stably maintained, making it a promising biological battery for ear implants.
Of course, this requires accessing the cochlea and connecting electrodes to the biological ‘anode’ and ‘cathode’ without interfering with normal ear function – no mean feat. But in a series of experiments with guinea pigs (as in actual research guinea pigs, not unwary humans), Stankovic and Chandrakasan pulled it off.
As Penders remarked, making electronics that can get by with what the body provides is a singular challenge, and the researchers here devised a custom semiconductor chip that can work with the approximately 1.1-6.3 nanowatts generated by the guinea pig EP – including a remarkable wireless radio transmitter that requires only 46 picowatts of standby power, and is estimated to be in ‘active mode’ only 0.0001% of the time. The initial test was only a proof of concept, showing that the chip could run and transmit a wireless signal for at least five hours continuously. Importantly, the authors observed some impairment of hearing, and note that:
“Our data imply that major improvements in low-impedance, small-diameter electrode design would be required to allow long-term energy extraction from the EP without causing long-term cellular trauma during electrode insertion.”
Nevertheless, it’s a very exciting demonstration both of sensor miniaturization and a promising potential mechanism for the long-term operation of cochlear implants and other inner-ear-based sensors in the future. Especially since most of the immediate challenges appear to relate to electrode miniaturization, an area where device manufacturers are making remarkably steady progress.
The second study, although more preliminary, is exciting because it’s targeted for use in cardiac pacemakers, which are the most widely-used medical implants currently on the market: according to a recent article in the American Heart Association’s journal Circulation, there are roughly three million people with implanted pacemakers worldwide. However, with a battery life of five to ten years, many patients can anticipate having to undergo replacement surgery at least once in their lifetime. As an alternative, M. Amin Karami of the University of Michigan is looking into piezoelectric harvesting – drawing power generated from vibrations. Last winter, Karami and his UMich colleague Daniel Inman published an article in Applied Physics Letters, describing how energy obtained from heartbeats might be transformed into a stable reservoir of long-term power for implanted pacemakers. More recently, they presented findings at the American Heart Association showing that their piezoelectric harvester, which is half the size of existing pacemaker batteries, could obtain ten times the power required to operate a pacemaker from the range of vibrations generated by a typical heart. Although these devices have not yet been put to the test in animal studies, this demonstration suggests a promising road forward for pacemakers as well as implanted defibrillators.
It’s definitely nice to think that there may be at least one aspect of our lives where bitching about lousy battery life might soon become a thing of the past – especially if it’s for technology designed to help keep us alive.